COVID 19 has brought us face to face with the need for disinfection 24/7.
Prior to COVID-19, most health care workers tolerated the role of an Infection Practitioner and the requirements imposed by the regulatory agencies. As a result of COVID, there are not enough ICP’s to meet the demand to track surveillance and adherence to proper techniques, let alone monitor handwashing. The lack of expertise available is felt in all areas of healthcare, from nursing homes to hospitals to clinics. Handwashing compliance has always been an issue with many avoiding the process deeming it cumbersome and time-consuming. COVID has changed the attitude of most HCW’s in the care of COVID patients, from the point of self preservation to protecting their patients.
Additionally, HCW’s have been bombarded with an onslaught of “solutions” addressing the disinfection of masks and face shields; gloving, double gloving, gowning, prepping rooms, etc. Solutions have ranged from the disinfection of masks, whatever their composition by UVC, heat, steam, peroxide vapor and other modalities. Many recommendations have been made with little science and little regard to the User and the safety of the devices after treatment. Little has been done with patient care devices.
“The effective disinfection of noncritical equipment and environmental surfaces is an important element in breaking the chain of healthcare-associated infections,” “ This equipment can serve as a mode of disease transmission as hospital personnel routinely touch noncritical equipment and then proceed to interact with and care for patients without necessarily changing gloves or washing their hands. This presents a significant opportunity for cross-contamination and potential infection.” (Baker, et al, 2015) ⁶
Joint Commission (JC) and Disinfection:
Traditionally Infection prevention is most often cited during JC inspections. The Infection Preventionist always take the brunt of the blame during these reviews.
New technology from TMG Health Technologies can make an impact on the two most cited standards as shown in the following tables. These findings are not unique to acute care and effect all health care facilities.
JOINT COMMISSION REPORT ¹: Annual Review 2020
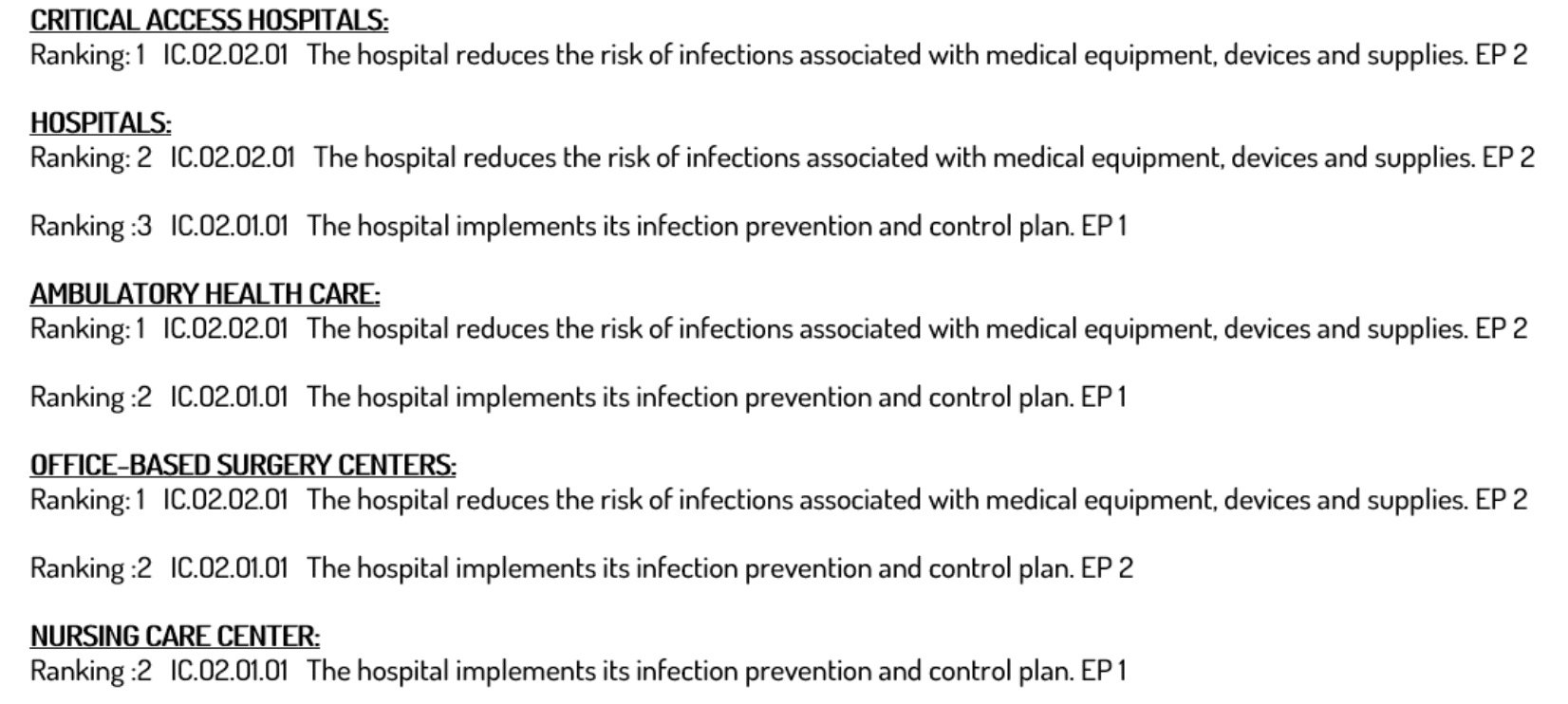
Although masks, gowning, and handwashing have precedence for protection of the healthcare worker, no attention has been paid to the multiples of patient-care tools and devices that are vectors for the spread of infections via touch, e.g. glucometers, stethoscopes, communicators, keyboards, transceivers, blood pressure cuffs, pumps and other point of care devices. The results of which are documented in the 2020 JC inspection report above.
If hands are washed but devices touched by those hands are not disinfected, little protection is gained.
Although COVID is primarily spread through droplets, other infections are passed by fomites as well as hands. The CDC documents that as much as 80% of infections are transferred by touch. ⁴ Simple Flu germs can last on hands for five [5] minutes and C. diff spores, MRSA and VRE for many days, which are then transferred to the very health devices and patient care tools used to keep patients safe.
In a 2017 published study documenting a quantitative assessment between hospitalized patients and portable medical equipment and other fomites, a total of 380 interactions between portable equipment or other fomites and patients were recorded. Of the 380 interactions, 156 (42 percent) involved equipment or fomites that made direct contact with the patient or surfaces in the room, including 128 of 316 (41 percent) on the medical-surgical wards and 28 of 64 (44 percent) in the ICU.
The researchers emphasized, “Our findings suggest that there is a need for protocols to ensure the effective cleaning of shared portable equipment.” ⁵
Studies
Studies have been performed using a variety of modalities including vaporized peroxide to disinfect certain unopened items in patient rooms while the room itself was being disinfected, (Otter, et al, 2013).³ In this study the dollars saved from recovered unopened patient supplies were significant approaching $400,000 in twelve months, associated with the patient discharges of twenty ICU rooms. The $400,000 did not include the saved cost from reduced waste disposal.
This peroxide robot without question is a means of achieving cost savings but requires the use of a modality that is time consuming, requires special skill and is not be available in many hospital systems. The cost of the vaporized peroxide robots is well over $120,000 for a basic unit with additional costs for recurring supply expenses. Being able to do this process throughout a system would necessitate the purchase of many robotic units, specially outfitted unoccupied rooms and the cost of personnel. The timing of room turnover is also impacted, not a good situation in the day-to-day operations of any hospital.
The preferred approach has been the use of UVC “RDS” [Rapid Decontamination System] cabinets to disinfect everything from a HCW’s personal effects, PPE, health electronics, non-critical medical tools and patient supplies. The rapid disinfection can be accomplished using a desktop sized “RDS” system that is mobilized on a cart to maximize its use room to room and department to department. As a closed system, there is no restriction as to where, when, who or how it can be used. Accessibility is the key. These systems are designed to be used 200 plus times daily by all medical staff. The more participants the greater the level of infection protection. TMG Health Technologies has placed numerous systems throughout healthcare and the government that routinely decontaminate hundreds of items and devices to a high level of efficacy in under 30 seconds with one-touch control. Independent studies have documented the systems performance in terminating COVID, MRSA, VRE, C. diff spores and other virulent pathogens.
In a national report on the “Top 10 Technology Health Hazards ²,” the ECRI Institute listed “Cleaning Fluid seeping into Electrical Components Can Lead to Equipment Damage and Fire.” A rapid UVC decontamination system, solves that problem. It is a totally “green” solution, requiring no chemicals, no heat, no moisture and no on-going supply cost to operate.
The national Association of Professionals in Infection Control and Epidemiology, {APIC}, reported that the number one challenge to achieve lower infection rates was the confusion on cleaning of complex portable equipment. The 30 second cycle time, the ease of use and the automated decontamination process providing a certified result, makes the “RDS” a must have infection prevention tool.
TMG Study
A recent study was performed by an independent laboratory to show the effect of the RDS system for the decontamination of soft packaging left in a patient room or surgical suite. Three different types of unopened original device packaging were streaked with 4 pathogens including MRSA, Group B strep, Pseudomonas, and Candida albicans. One and one-half million [1.5 million] of organism were streaked onto the packaging, top and bottom and placed into the RDS unit at cycles of 30, 60, and 90 seconds. The streaks were then swabbed and plated on blood agar for each time period. All of the packaging resulted in a > 6 log₁₀ reduction on colonies in a single 30 second cycle, validating the efficacy and the simplicity of this cost-effective, easy to deploy, automated solution for the decontamination of unused, unopened packaged medical supplies, resulting in great savings.
As mentioned in the Otter paper, the US throws out millions of dollars of unused patient medical supplies from hospitals. These supplies are routinely discarded upon patient transfer or discharge simply because that was the norm. The ICU’, NICU, ER and OR are notoriously guilty of overstocking. Many attempts have been made to try and control inventory, but in these crisis areas no one has the time to search for inventory and there was no incentive to save. It is doubtful that the average HCW has savings on their mind, but managers and CFO’s do.
The cost of the UVC “RDS” like most top end systems providing high level disinfection would appear to be a challenge, except for the fact that the same “RDS” units are used to decontaminate unopened items in a patient’s room, returning them to inventory for a real and immediate dollar-for-dollar cost savings to the department.
Facilities that have deployed this strategy have experienced a double-digit return-on-investment in the first thirty [30] days. Facilities both small and large have “RDS” units in quantities of two [2] to sixteen [16]. For the same cost as a single UVC Mobile Robot or HPV system, a 350 hospital could acquire a “RDS” Rapid UVC Decontamination system for every department in the hospital. The cost savings in reduced infections, supply inventories and reduced waste disposal costs provides an immediate ROI. Real dollars under your control, resulting in an immediate impact to the bottom-line.
TMG Disinfection Support
TMG supports the concept of disinfection for all items used by a healthcare worker and is willing to share the numbers and provide the guidance to initiate a personalized program for you. Lowering the chance of infections and cross-contamination on shared tools and devices should be paramount in a hospital’s overall strategy to protect HCW and patients. The Joint Commission Report dated May 12, 2021, confirms this.
The Plan
Find out how to make this happen in your healthcare environment! TMG can help. They have a team of health practitioner’s that have been there and done that. It’s a proven process with demonstratable success at facilities small and large. The implementation time is less than 30 days. The next step is yours. Disinfection of patient care items as well as HCW personal items will lower transmission of pathogens and support handwashing compliance. Regulators view this as beneficial to the patient and environment of care regulations.
Demonstrating a consistency of practices will lower the burden of HAI transmission throughout a healthcare system. The lack of Infection control planning is a challenge documented in the cited Joint Commission Standards of May 12, 2021.
Packaged supply waste has been a documented practice written about for years with estimates in the $Billions of dollars. ⁷ Yet cost-containment continues to be a top priority goal of every healthcare executive, now more than ever. ⁸
The success of the facilities that have implemented the “RDS” program, have proven that both goals are within reach.
References:
1. Joint Commission On=Line, May 12, 2021:
https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/joint-commission-online/may-12-2021/top-5-mostchallengingrequirements-for-2020/
2. ECRI: Top Ten Technology Hazards 2019: https://www.mlmic.com/blog/physicians/ecri-health-technology-hazards-2019
3. Otter, JA et al, Infect control Epidemiology 2013;34(5): 472-478
https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/abs/saving-costs-through-the-decontamination-of-thepackaging-of-unused-medical-supplies-using-hydrogen-peroxidevapor/5A9ADBFC1EC771D47A04CB121DCA09CF
4. CDC : 80% of Infections Are Spread by Hand.
https://www.cdc.gov/infectioncontrol/guidelines/environmental/index.html
5. Quantitative assessment of interactions between hospitalized patients and portable medical equipment and other fomites. DOI: https://doi.org/10.1016/j.ajic.2017.05.003
6. Baker, R., Macks, V.,Hilliard, P.(2015) Reprocessing noncritical equipment: Assessment and Technology Improves Infection Prevention Practices (May 7,2015). Infection Control Today,
http://www.infectioncontroltoday.com/environmental-hygiene/reprocessing-noncriticalequipment-assessment-and-technology-improves
7. What Hospitals Waste, A look at all the perfectly good stuff hospitals throw away. Marshall Allen, ProPublica,
https://www.propublica.org/article/what-hospitals-waste
8. Annual Health Care CEO Survey: Cost Control is Top Priority for Hospital Executives; Business Wire
https://www.businesswire.com/news/home/20180711005184/en/Annual-Health-Care-CEO-Survey-Cost-Control

